Female Fertility Treatments
There are a wide variety of female fertility treatment options available. This website section provides an introduction to these fertility interventions from the female side as well as their relationship to male fertility potential. There are many good online and print resources you can consult, and a specialist in female fertility is an excellent source of information as well.
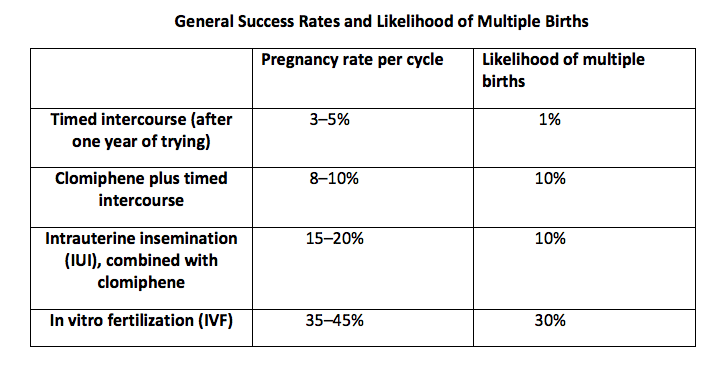
The above chart shows approximate rates of pregnancy and the chance of multiple births for different treatments. These are general numbers; your specialist can provide you with more individualized estimated success rates that take into consideration your particular circumstances.
Female Fertility Medications
Hormonal medications such as clomiphene (Clomid), tamoxifen (Nolvadex), letrozole (Femara), and anastrazole (Arimidex) are often effective in treating ovulatory dysfunction, with the goal of reestablishing normal ovulation. In women with otherwise normal ovulation, these medications can also (modestly) increase the chance of pregnancy by producing a higher number of eggs than normal. This type of medication is generally taken for about five days, starting between day 3 and day 5 of the woman’s cycle. They are inexpensive (generally costing under $50 per cycle), but do increase the risk of multiple births (up to 10 percent chance of twins, with less than 1 percent chance of triplets or other higher-order pregnancies). For the best chances of success, a total motile sperm count of at least 20 million is desirable when using natural intercourse combined with medications, though men with lower total motile counts may be successful as well.
General ob-gyns often feel comfortable prescribing medications like clomiphene. If three or four cycles of these medications do not result in pregnancy, the chance of success with additional cycles starts to decrease significantly , and women are typically encouraged to think about moving on to other treatment options, such as intrauterine insemination.
Other hormone treatments include human chorionic gonadotropin injections which are sometimes used to "release" an egg from the ovary at an appropriate time. FSH (follicle stimulating hormone) can also be used to drive ovaries to make large numbers of eggs.
Intrauterine Insemination
Also known as artificial Insemination, intrauterine insemination (IUI) involves placing the man’s sperm directly into his partner’s uterus at the correct time during her ovulatory cycle. A woman undergoing IUI is often given medications such as clomiphene, although natural-cycle IUI can be performed without any medications. The addition of medications can increase the chances of success modestly, but it also increases the risk of multiple births (to about 10 percent).
The woman is generally monitored by blood tests or intravaginal ultrasound, and at the time of her peak fertility, just before ovulation, the man is asked to give a semen sample. The sperm are processed (washed and concentrated) and placed into the woman’s uterus through a slender tube; this is typically not much more painful than a Pap smear.
A minimum of 5 million pre-wash total motile sperm or 1 million post-wash total motile sperm is needed for a decent chance of success; higher total motile sperm counts do increase the chances of pregnancy. Sometimes double collections are performed to increase the number of sperm that are inseminated. Some reproductive endocrinologists recommend natural intercourse either right before or right after an IUI as well. Pooling of multiple frozen semen specimens for IUI can be performed, but in general 50 to 75 percent of the sperm from each sample do not survive the freeze/thaw process, so fresh specimens are best when they are available.
Some general ob-gyns perform IUI in their office. However, most ob-gyns prefer to refer women to a fertility specialist for insemination.
Cost of IUI
The cost for IUI ranges between $400 and $1,600 for each cycle.
Intrauterine Insemination with Gonadotropins
IUI can be combined with the use of gonadotropins by the woman in order to generate a larger number of eggs. This is associated with higher pregnancy rates, but the trade-off is increased risk of multiple births as well as cost—the hormonal medications can be expensive. The chance of higher-order births (triplets or more) is significantly higher when IUI is combined with gonadotropins, since there is no control over the number of eggs that are released and potentially fertilized within the woman’s reproductive tract.
In Vitro Fertilization
Standard in vitro fertilization (IVF) involves extracting eggs from the woman and mixing them directly with sperm in the lab. A variant of this, called intracytoplasmic sperm injection (ICSI), involves injecting a single sperm into each egg. Fewer sperm are required for ICSI, making it the procedure of choice for men who can only produce small numbers of sperm. ICSI can also bypass problems with egg/sperm interactions, and is recommended for men with very low strict morphology readings (under 3–4%) and for couples who have had multiple failures with standard IVF for unknown reasons. ICSI is also used when testicular or epididymal sperm extraction was necessary to retrieve sperm.
In both standard IVF and ICSI, the woman is injected with medications that increase the number of eggs she produces in each cycle. The eggs are removed under transvaginal ultrasound guidance and combined with the sperm. After the fertilized eggs (now called embryos) have been allowed to mature for a few days, two to four embryos (depending on factors such as the woman’s age, the quality of the embryos, etc.) are transferred into the woman’s uterus. Any remaining embryos can be frozen for later use.
IVF protocols are constantly being modified to improve outcomes. Current trends include the transfer of only one embryo (called single embryo transfer). Already common in Europe, this practice has the potential to dramatically decrease the number of higher-order pregnancies, but it has the trade-off of a potentially lower pregnancy rate per cycle. Some institutions are also using an approach in which they freeze all embryos and then transfer them to the woman later, when the uterus has returned to a more normal physiologic environment (as opposed to the hyperstimulated state that a fresh embryo is transferred into); potential benefits in terms of pregnancy outcomes as well as the future health implications for the embryo and baby are being investigated.
There are a number of common concerns associated with IVF:
1) Cost. IVF is expensive, with a typical cycle costing between $10,000 and $15,000.
2) Increased risk of birth defects. The vast majority of babies born to couples undergoing IVF are normal, but there is some evidence that rates of rare birth defects are higher than in natural pregnancies. It is unclear whether this slightly elevated risk is due to changes in the woman’s hormonal environment, loss of the egg’s natural selection process of excluding defective sperm (with ICSI), or some other factor.
3) What to do with unused frozen embryos. Several options exist, including embryo donation.
4) Hyperstimulation. A small number of women create too many eggs during the stimulation phase, which can lead to potentially serious complications and hospitalization.
Your female fertility specialist can provide you with more information about each of these concerns, as well as strategies to navigate these potential problems.
IVF Outcomes
The Society for Assisted Reproductive Technologies (SART) is a national professional organization that provides information to both patients and medical providers regarding the IVF process. SART also reports IVF outcomes for almost all of the IVF programs in the United States, with a lag time of several years (to accumulate and process the data). The SART website (www.sart.org) contains a map listing the IVF programs in each state, as well as the statistics of that program’s IVF outcomes based upon a number of factors, including the woman’s age.
Preliminary nationwide data from 2014 (the most recent available) from SART are shown below. The numbers indicate the live birth rate after a cycle was initiated for egg retrieval, and includes all embryos transfers (fresh and frozen) derived from that cycle.
Age of the Woman (Yrs): <35 35-57 38-40 41-42 >42
Live Birth Rate (%): 48.7% 38.2% 24.3% 12.3% 3.7%
Typical IVF Cycle
Here’s how a typical cycle of IVF works:
1) The woman takes an oral contraceptive for fourteen to twenty-one days, starting on day 4 of her menstrual cycle. This reduces the chance of hyperstimulation and ovarian cyst formation. Women who have decreased ovarian reserve usually skip this step.
2) A GnRH agonist (such as Lupron) is taken for twelve to fifteen days. This temporarily shuts down the ovaries, preventing premature ovulation and ensuring that all of the eggs for this cycle mature at the same time.
3) A gonadotropin (e.g., Gonal F) is administered for ten to twelve days, to stimulate ovarian egg production. During this period the woman is monitored regularly with ultrasound and blood tests.
4) An injection of human chorionic gonadotropin (HCG) is given, to cause final maturation of the eggs.
5) The eggs are retrieved, generally around thirty-six hours after the HCG injection.
6) The eggs are fertilized in the lab and allowed to mature for three to five days.
7) The embryos are transferred to the woman’s uterus, and progesterone is administered to support implantation.
8) A pregnancy test is done fourteen days after retrieval or transfer.
9) If pregnancy results, two ultrasounds are done: the first either two weeks after a positive pregnancy test or at 6.5–7.5 weeks of pregnancy, and the second at 7.5–8.5 weeks of pregnancy.
10) After 8 to 10 weeks of pregnancy, the woman’s care is transferred from the specialist back to her regular ob-gyn for the remainder of the pregnancy.
This is only a rough guide; your particular IVF cycle may proceed somewhat differently, based on your fertility specialist’s preference, the particular clinical situation, and how the cycle is progressing.
IVF Terminology (by Day of Cycle)
Day 0: Egg retrieval
Day 1: Fertilization
Day 2: Cleavage to 2-cell stage
Day 3: 8-cell stage
Day 4: Morula stage (around 30 cells)
Day 5: Blastocyst stage (generally 50–150 cells)