The Impact of Antioxidants and Oxidative Stress on Sperm Quality
Elevated levels of oxidative stress are a common and important cause of male infertility problems, including sperm quality and elevated levels of sperm DNA fragmentation. The elimination of oxidative stress risk factors as well as the use of supplementation of antioxidants have been shown to have the potential to improve male fertility as well as the outcomes of treatments including IVF.
OXIDATIVE STRESS AND ANTIOXIDANTs - an introduction to their relationship with male fertility potential
Oxidative stress is an important contributor to male infertility problems. Studies have shown that between 30-80% of men with fertility problems have elevated levels of oxidative stress. [Kuchakulla M. Urology 2019] This section of the website will review the causes, possible testing, and management options for the management of oxidative stress.
WHAT IS OXIDATIVE STRESS?
The body’s normal metabolic processes create by-products called reactive oxygen species (ROS), also called free radicals. These metabolic by-products have the potential to negatively affect individual cells, tissues, and organs, but under normal circumstances the body is well equipped with antioxidants, substances that mop up excess reactive oxygen species before significant problems occur. Small amounts of ROS are normally present within the genital duct system, and in fact they are thought to play an important positive role in normal sperm production and function.
However, when the amount of ROS becomes greater than the body’s normal cleanup mechanisms can easily handle, the result is increased oxidative stress on the body. Unfortunately, sperm are especially sensitive to oxidative stress, which can result in cellular and DNA damage and lead to decreases in both sperm numbers and quality.
IF OXYGEN IS DAMAGING TO CELLS, WHY DOES THE BODY USE IT?
The human body’s relationship with oxygen is complicated. The first life forms on the planet were anaerobic and did not utilize oxygen in their metabolism. However, the use of oxygen within the body increases the energy available for use by its cells 20-fold, and aerobic metabolism allowed an explosion of development within the animal kingdom leading the great diversity of organisms that we see today. However, there was a price to pay for this increased energy. When oxygen loses one of its molecules during the course of natural body chemical reactions, it becomes a reactive oxygen species which are damaging to cells. Over time, organisms have found ways of effectively limiting the effects of oxidative damage while keeping the energy advantages of oxygen use. The use of natural antioxidant mechanisms is widespread throughout the body and help to neutralize the negative effects of oxidative stress on the body.
Unfortunately, sperm are particularly vulnerable to the damages of oxidative stress. Sperm have a specific job which requires them to be compact and mobile for their long journey through the female reproductive tract. While their ability to swim efficiently is helped by their compact structure, what is sacrificed are antioxidants and a built-in ability to repair damage from oxidative stress. Their high levels of polyunsaturated fatty acids also make sperm vulnerable to damage from oxygen free radicals as well. Multiple studies have linked elevated levels of oxidative stress to decreased semen parameters such as density and motility. [Tremellen K. HumReprodUpdate 2008][Agarwal A. Fert/Steril 2003]. Oxygen free radicals are also felt to have the ability to damage the sperm DNA and elevated levels of sperm DNA fragmentation (DFI) have been noted in men with oxidative stress. [Gharagozloo P. HumReprod 2011]
CAUSES OF INCREASED OXIDATIVE STRESS
There are many reasons why a man can be experiencing increased oxidative stress. These include:
1) Pyospermia- One reason for increased levels of ROS in the genital duct system is the presence of higher-than-normal levels of white blood cells, which can be a sign of infection or inflammation. Pyospermia is the term for semen that contains elevated levels of WBCs.
2) Increased numbers of immature sperm cells- immature sperm are found in increased numbers in men with decreased sperm counts and these immature cells generate more oxygen free radicals than their mature counterparts. may be another cause of oxidative stress.
3) Significant illness or stress on the body
4) Extremely strenuous physical activity
5) Increased scrotal temperature
6) Varicoceles
7) Lifestyle choices- including tobacco products, marijuana and other illicit drugs, excessive alcohol intake
8) Exposure to chemicals, air pollution, and pesticides
TESTING FOR OXIDATIVE STRESS during the male infertility evaluation
There are several different ways to try and measure oxidative stress levels in the male genital duct system. However, measuring oxidative stress is not at this time considered a routine male fertility test in most clinical practices. Since antioxidant regimens are not very expensive and have minimal side effects in most men, many clinicians just choose to start all of their male fertility patients on antioxidants, thus eliminating the cost and time of antioxidant testing. However, some clinicians do routinely check for levels of oxidative stress in the semen of male infertility patients. Others reserve this testing for special circumstances, such as men with persistent pyospermia (elevated white blood cells in the semen) despite adequate antimicrobial and anti-inflammatory therapies. See "Reversible Semen Analysis Factors" for more information on pyospermia.
Many different methods for testing oxidative stress (ROS) in cells exist, including chemiluminescense and colorimetric assays, thiobarbituric acid, and annexin V. However, from a practical standpoint, sperm oxidative stress testing is generally performed by the oxidative stress adduct (OSA) test, as well as the MiOXSYS system.
ROS OF SEMEN
Tests the amount of reactive oxidative species (ROS) within the semen. These generally are measured indirectly, by the ability of the semen to absorb the potentially damaging free oxygen radicals. Generally, these tests measure the total antioxidant capacity of the seminal plasma.
OXIDATIVE STRESS ADDUCT TEST
A specialized test, called the oxidative stress adduct (OSA) test, can directly measure the degree of oxidative damage to the sperm. OSA testing is available from Reprosource (www.reprosource.com) and is part of the company’s Advanced Semen Report, which also includes DNA fragmentation index testing.
For the oxidative stress adduct (OSA) test, a normal result is under 3.8, a borderline result is between 3.8 and 4.4, and an abnormal result is over 4.4.
For cost information on the OSA test, please see the "Genetics and Advanced Sperm Testing Costs" section of this website.
MIOXSYS TEST
This is a test developed at the Cleveland Clinic. The supposed advantage of the MiOXSYS test is that it evaluates both the number of oxidants in the semen (like the ROS test) as well as the amount of oxidative reductants present (which eliminate oxygen free radicals). There are also other supposed advantages in terms of cost of testing, amount of specimen needed to be tested, and the ability to evaluate both fresh and frozen specimens. Tests results are reported as oxidation reduction potential (ORP) in 2 ways:
1) Static ORP (sORP)
-sORP measures the current balance between total antioxidants and reductants and is measured in millivolts (mV).
2) Antioxidant capacity reserve (cORP)
-cORP measures the semen’s antioxidant potential, measured in micro-coulombs (µC)
Semen levels of ORP as reported in a recent study [Agarwal A, et al. Fertility and Sterility 2016]
Men with normal motility Men with low motility
sORP 2.55 35.28
cORP 1.71 3.49
The MiOXSYS is available through AYTU BioScience Inc. which sells the testing device to specific fertility labs. Availability and pricing are going to vary regionally.
SUMMARY OF OXIDATIVE STRESS TESTING
There are no specific guidelines on the performing of oxidative stress testing. Four possible clinical uses for oxidative stress testing:
1) For physicians who use these tests to guide which patients should be started on antioxidant supplements.
2) Patients who are having trouble with certain fertility risk factors, such as smoking cessation, to see if there is some objective evidence that this risk factor is causing on-going problems with fertility potential.
3) Evaluation for the presence of male factor problems in men with normal semen parameters, since elevated levels of oxidative stress are often associated with decreased fertility potential. For example, a man who has been unable to conceive for a year who has normal semen parameters but smokes cigarettes. An elevated level of oxidative stress may be an indicator that male factor issues may be contributing to their inability to conceive despite normal semen parameters. This man may benefit from smoking cessation and/or antioxidant supplements.
4) A man with persistent pyospermia that is resistant to treatment, since pyospermia can be associated with increased oxidative stress on sperm. The presence or absence of elevated oxidative stress could potentially provide information about whether the sperm are still experiencing oxidative stress despite antioxidant therapy, in which case sperm wash and IUI may be helpful.
MANAGEMENT OF OXIDATIVE STRESS to optimize semen parameters
Managing oxidative stress in men generally takes two approaches
1) Eliminating oxidative stress factors where possible
2) Supplementation with antioxidants
ELIMINATION OF OXIDATIVE STRESS FACTORS
These include:
1) Treatment of pyospermia (elevated levels of white blood cells in the semen)
2) Avoiding sperm toxins (e.g. elevated heat exposure, tobacco use, work-related and environmental toxins)
3) Evaluation for varicoceles (dilated veins in the scrotum)
ANTIOXIDANTS
CLINICAL IMPACT OF ANTIOXIDANTS
A fairly large number of studies have evaluated the ability of antioxidants to improve semen parameters and fertility outcomes. The difficulty in evaluating the data is that many of the studies are small and not controlled (i.e. not double blind, placebo controlled). Also, since there are such as wide variety of antioxidant supplements available (each containing different amounts of active ingredient), the studies inevitably include a wide range of treatment regimens, making it difficult to decipher which of the antioxidants may be offering more benefit than the others.
As a general statement, reviews of the literature have found a beneficial impact of the use of antioxidants on reversing the damages of oxidative stress on sperm. [Majzoub A. ArabJUrol 2018]. Improvements in semen parameters and live birth rates following natural intercourse have been noted. [Safarinejad MR. JUrol 2009][Keskes-Ammar L. ArchAndrol 2003] Improvements in sperm DNA fragmentation levels have been documents with antioxidant use. [Salehi P. IntJReprodBiomed 2019]. Even with advanced female treatments such as IVF/ICSI are used, improvements in fertility outcomes have been noted. [Greco E. HumReprod 2005][Tremellen K. AustNZJObstrGyn 2007]. Overall, most studies of antioxidants have shown improvements in semen parameters and decrease levels of sperm DNA fragmentation, but not all of them. [Alhaman A. FertSteril 2023]. The 2020 MOXI (Males, Antioxidants, and Fertility) trial randomized 171 infertile men to either an antioxidant regimen (Vit C, E, selenium, L-carnitine, zinc, folic acid, and lycopene) or placebo. After 3 to 6 months, there was no significant improvement in sperm density, motility, DNA fragmentation, or pregnancy and live birth rates with either natural intercourse or IUI. [Steiner A. FertSteril 2020]. There is some concern as well that taking too many antioxidants can also potentially have a detrimental impact on a man’s general health and fertility outcomes as well, so “more” is not necessarily better. [Henkel R. Andrologia 2019]
Conclusion
A Cochrane review of the available literature in 2014 found a statistically significant improvement in pregnancy and live birth rates in couples where men were taking a regimen of antioxidants. These findings have been questioned by more recent studies such as the relatively small MOXI trial. Clearly, larger randomized trials which contain all of the supplements felt to potentially beneficial (the MOXI trial did not include CoQ10) are needed to better elucidate the impact of these therapies on fertility outcomes. Until that time, the majority of evidence seems to point to a potential benefit of antioxidants in the management of male infertility. No specific antioxidant formula has been proven to be more effective than the others in clinical trials. Relatively cost-effective options are available, and the use of basic antioxidants seems to be safe in most men if excessive amounts are not used.
APPROACHES TO USING ANTIOXIDANTS IN MEN
There 3 main approaches that clinicians can use for antioxidants in managing male infertility:
1) Recommending antioxidants for all men with fertility issues
2) Reserve antioxidants for men who have certain significant risk factors (such as tobacco use or pyospermia)
3) Only use antioxidants if elevated levels of oxidative stress are found upon testing (as discussed above)
None of these approaches has been proven superior at this point in time. As mentioned earlier, the use of antioxidants does not need to be very expensive and is generally low risk in most men if used properly. However, there is the small risk of an idiosyncratic reaction to any supplement. Also, some men go overboard and take the “more is better” approach to antioxidant supplements which can potentially lead to decreased fertility and potential health implications. Therefore, some male fertility specialists prefer to reserve antioxidants for those men who have certain risk factors for increased risk of oxidative stress, or who have proven to have signs of this on semen testing.
WHICH ANTIOXIDANT INGREDIENTS TO USE
There is a bewildering array of antioxidants available on the internet today and choosing which ones to use can be difficult. A 2019 review of the available data on common antioxidants for male infertility found that the effectiveness of most antioxidants that are commonly used has not been well studied. Only 22% of the ingredients reviewed had published data on their impact on semen parameters and pregnancy outcomes, and a mere 17% showed improvements through their use. [Kuchakulla M. Urology 2019]. The 6 ingredients with the best evidence were:
1) L-Carnitine
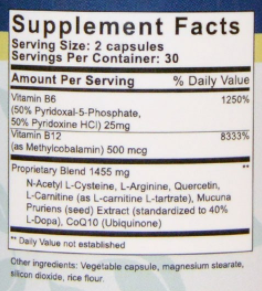
2) Co-enzyme Q (CoQ10)
3) Vitamin E
4) Vitamin C
5) Vitamin D
6) Zinc
Minimal evidence for improvement was found with selenium, Maca root and Vit B12.
Coenzyme Q10 (CoQ10)
Also known as ubiquinone or ubiquinol, CoQ10 is a vitamin-like substance that has antioxidant properties and is also involved in cellular energy production. Studies have associated CoQ10 supplementation with improvements in semen parameters, though the literature has not to date documented a definitive improvement in pregnancy rates.
L-carnitine
L-carnitine is an amino acid (a building block for proteins) that has antioxidant properties and is also involved in cellular fatty acid metabolism. Supplementation of L-carnitine has been associated with improvement in semen parameters (especially motility).
L-Carnitine and Cardiovascular Risk
Research from the Cleveland Clinic has linked L-carnitine intake to increased cardiovascular risk factors, alongside fat and cholesterol. L-carnitine is found in high levels in red meat. When consumed by people who regularly eat red meat, L-carnitine can be broken down by intestinal bacteria into TMAO, a by-product that can lead to increased atherosclerotic vessel damage. Interestingly, vegetarians may not have the necessary bacteria in their intestines to break down L-carnitine into TMAO. More research is certainly needed on this topic. My current take on the subject is this: L-carnitine may modestly increase cardiovascular risk if taken over long periods of time. I therefore only recommend that men take L-carnitine while they are trying to achieve a pregnancy. Once their partner is pregnant, I recommend that they stop all fertility-related supplements. Men who have a strong personal or family history of cardiovascular disease should discuss L-carnitine use with their cardiologist or primary care physician before starting this supplement.
Zinc
Zinc is a mineral that is found in large concentrations within the epididymis. Though having no antioxidant properties itself, zinc assists with the antioxidant actions of some enzymes. Some studies have correlated lower sperm quality with decreased zinc levels, though others were inconclusive. The daily recommended intake of zinc for men is 11mg per day.
RELATIVE EFFECTIVENESS OF DIFFERENT ANTIOXIDANTS
A wide variety of male fertility supplements are available to men. There is essentially no good evidence evaluating the clinical efficacy as well as safety of the different commercially available antioxidants regimens currently available on the internet.
As per the 2019 Kuchakulla study described above, there is decent evidence to suggest that any antioxidant regimen that you use should contain at least the following components. The dosages listed were not tested in this study but are general daily recommended dosages commonly used with these supplements:
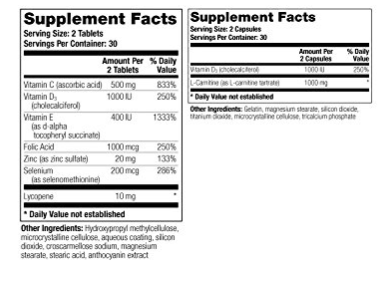
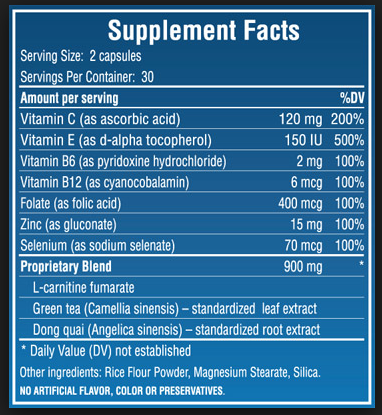
1) Vitamin C: 250 mg
2) Vitamin E: 200 IU
3) Vitamin D: 1000 IU
4) Zinc: 7.5 mcg
5) L-carnitine: 500 mg once a day (or 1,000 mg every other day)
6) Coenzyme Q10 (CoQ10): 200 mg once a day (or 400 mg every other day)
In order to get a regimen containing these ingredients, you have 3 options. One is to take a multivitamin pill which contains the first 4 ingredients and then add an L-carnitine and CoQ10 pill each day as well. A second option is to find a commercially available supplement which contains all 6 of the ingredients. The third is to find a commercially available supplement which has some, but not all, of the 6 ingredients, and supplement the missing elements.
Note on Supplements and Dosages: the above listed dosages are general recommendations of minimum amounts that may benefit fertility potential in men. These are approximations for the general population, and there is not solid scientific data to back up these specific amounts. Also, final decisions on dosages should be made with your medical provider, as some men with certain medical conditions or taking certain medications may need to modify their intake accordingly.
Once a pregnancy has been established, I generally recommend that the supplements should be discontinued.
COMMERCIALLY AVAILABLE SUPPLEMENTS
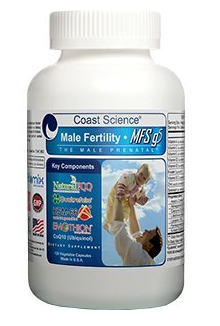
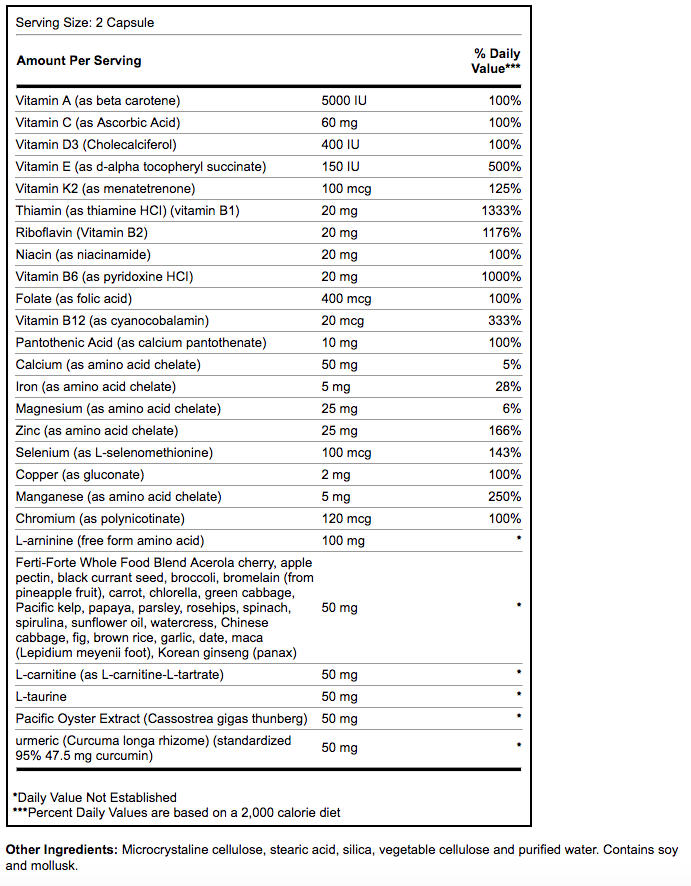
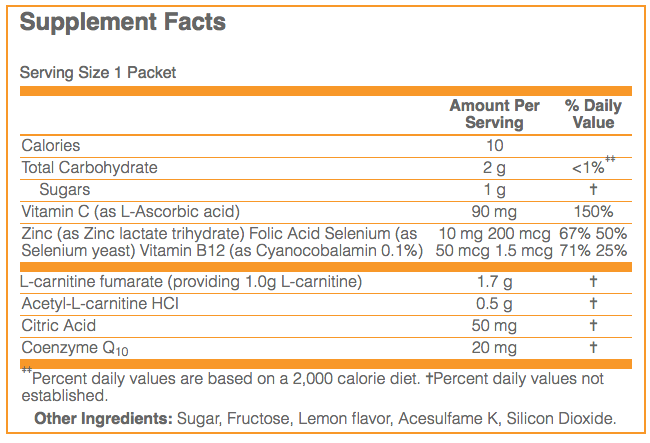
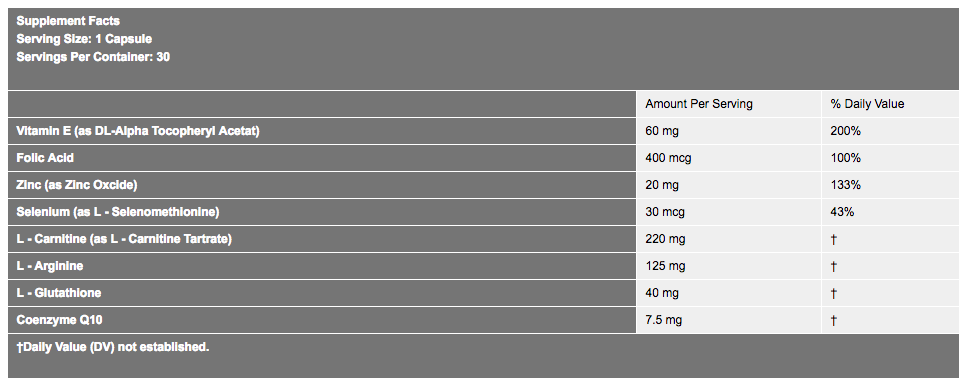
The following is a list of commercially available supplements (in alphabetical order) in a chart which contains their relative quantities of 8 common ingredients that are often used for male infertility. Some supplements do not list the amounts of L-carnitine and/or Co-enzyme Q, but just have them listed as part of a "proprietary blend" making comparisons with other supplements difficult. Of note, most supplements have additional ingredients beyond the 8 on the chart, which may or may not assist with male fertility potential. We have included the product labels below for each of the listed antioxidant supplements below so that you can review the full list of ingredients. The pricing is based on an April 2020 survey, primarily from Amazon.
[Note: We try to keep this information as accurate as possible for each supplement, but sometimes errors are made in transcription or formulations are changed. So that we can keep our information as accurate as possible, please contact us with any corrections/updates either in our "Comments" section (link at the bottom of this page) or by email at maleinfertilityguide@gmail.com.]